Charting Your Cervical Position
This is the most challenging fertility sign for many women, and it might take a few cycles to figure out the differences in how the cervix feels during certain times of your cycle.
When ovulation is near, your cervix tends to rise, soften (similar feeling to your lips), and open in preparation for conception. At other times of the month, the cervix will be lower and firmer, like the tip of your nose. To chart cervical position, insert a clean middle finger inside yourself, and note what you feel. If you are charting your fluid and temperature and getting less than obvious results, (a change in your cervical fluid and a thermal shift are not leading to obvious signs of ovulation), having this third piece of information can be helpful.
● Start charting your cervical position once a day after your period ends
● Make sure your hands are clean, and your fingernails are trimmed
● Try to check around the same time each day
● If you have already experienced childbirth (vaginally) your cervix will always be slightly open, and more oval in shape
● If you notice small bumps, like sand, no need to worry! These usually come and go on their own
● Once you become more familiar with how your cervix feels throughout your cycle, you may limit your charting to when your fertile quality fluid begins until your thermal shift
● Most women find it is easiest to find and check the cervix in a squatting position. When you first start out, finding the cervix after ovulation when the cervix is firm and low. Over time, you will begin to notice the elevation, softening and opening of the cervix that happens just prior to ovulation
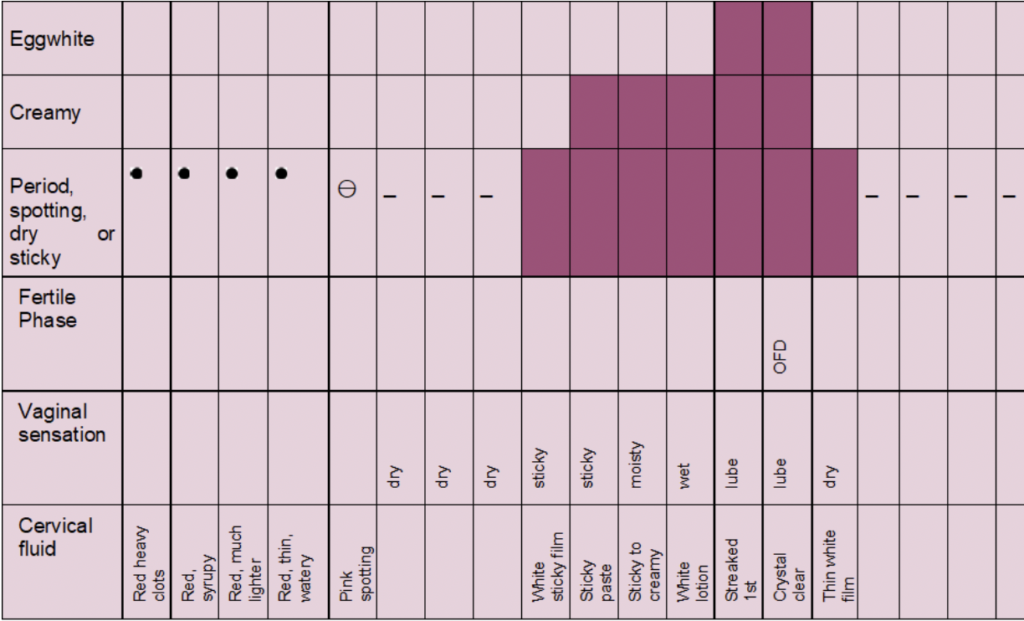
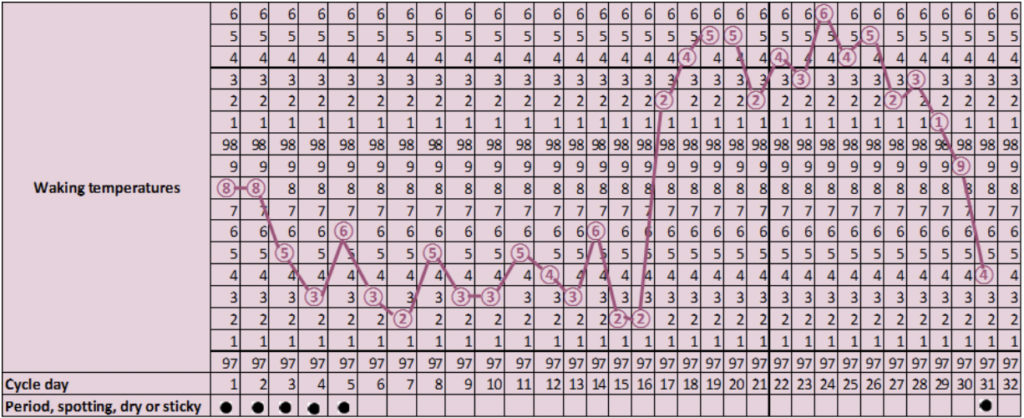
Length of Your Luteal Phase
The luteal phase of your cycle is the time from ovulation until your next period begins. It starts with the day of your thermal shift, and ends the day before your next period starts.
You count through the last day before your period, even if there is a thermal shift a day before or you have blood spotting. However, if your thermal shift always occurs more than 2 days after your Optimal Fertility Day, then it means that your body reacts slowly to the progesterone released after ovulation. In that case, you count as the first day of your luteal phase the day after your Optimal Fertility Day.
A typical luteal phase usually lasts 12-16 days, but it may be as short as 10 days. If it’s less than 10 days, that’s generally considered too short. A short luteal phase can cause problems with conception because the body doesn’t have time to grow a healthy uterine lining which is critical for implantation of the fertilized egg. If the egg does not find a suitable environment in which to grow, it cannot thrive, your period starts, and you have early loss of a pregnancy. Some women with consistently short luteal phases may repeatedly get pregnant and miscarry without even knowing it since their period comes on time or very close to it -seems like a normal period- and pregnancy is never identified.
Women may experience an inadequate luteal phase where their temperature rises after ovulation but only slightly due to inadequate amounts of progesterone being produced. In other women, their temperature falls off quickly after an adequate rise following ovulation indicating that adequate amounts of progesterone are produced but not for a long enough period of time to maintain successful implantation of a fertilized egg.
If you determine you have a short or abnormal luteal phase through temperature charting- seek the advice of your physician. Work up should include a progesterone level around day 21 (or approx. 7 days after ovulation), or a pooled progesterone level (taken on the day of ovulation plus days 3, 5, 7, 9 and 11 after ovulation) and a prolactin level to rule this out as a cause. Options include progesterone therapy during the second half of the cycle or Clomid therapy.
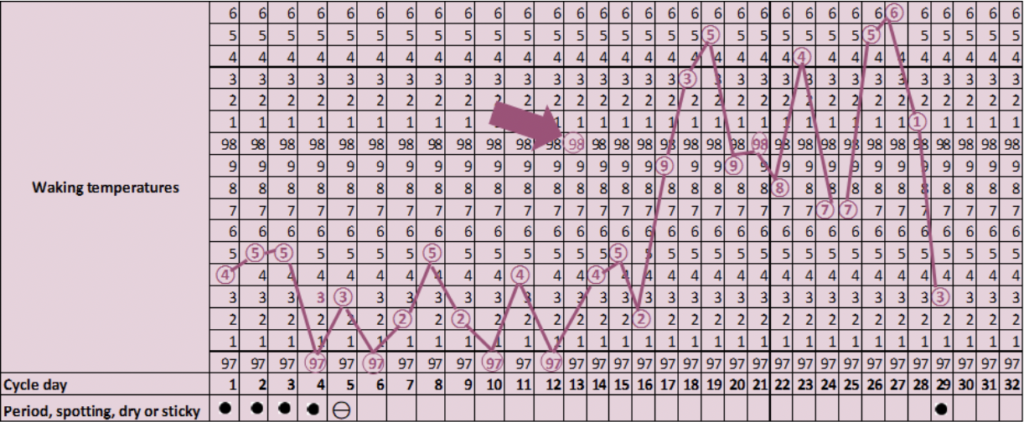
Coming Off the Pill and Other Hormonal Methods
A woman’s cycle tends to be more exact or regular on birth control pills vs off of birth control pills because bleeding is controlled through the synthetic hormones in the birth control pill. After the pill is stopped, you may find that your cycles are irregular for a period of time and/or may return to whatever pattern of bleeding you had prior to starting the pill. If you had menstrual irregularity prior to starting the pill, you can likely expect that your cycles will be irregular once again off the pill. There are a variety of patterns a woman can see after discontinuation of birth control pills which include:
- High or low temperatures
- Temperatures that do not match with the cervical fluid you are making
- Little or excessive cervical fluid, of unusual consistency
- Heavier or lighter bleeding than when you were on the pill
- Spotting during the luteal phase of your cycle or prior to menstruation
- Short luteal phases
All of this varies from woman to woman. Some women get their cycles back relatively soon after coming off the pill, while others it can take up to a year or two. And even when a cycle returns and seems relatively normal, important signs that indicate health and optimal balance may still be missing. For example, a woman may experience short luteal phases for the first few months, making fertilization possible but successful implantation difficult. It’s recommended to discontinue the use of hormonal birth control at least 3-6 months prior to your desired conception date.
What About Ovulation Predictor Kits (OPKS)?
An OPK detects the occurrence of the luteinizing hormone (LH) in the urine, which surges before ovulation. Therefore, it can provide an estimation on when you may approaching ovulation. However, as the kit only measures the LH surge, its results can be misleading for various reasons, as discussed below:
- The kit can estimate the time of ovulation but cannot determine if ovulation occurred. Women with LUFS (luteinized unruptured follicle syndrome), experience an LH surge but an egg is never released, in other words, they do not ovulate.
- Women suffering from PCOS (Polycystic Ovarian Syndrome) experience many spikes in their LH levels, thus the ovulation kits can provide misleading results.
- Women close to menopause have increased LH levels, which can cause the kit to provide false results. In general, the kit should show only one day of the LH surge. If the kit indicates more than one day, then the results are probably invalid.
- Women whose LH surge lasts less than 10 hours and use the kit once a day, may miss their LH surge.
- Women whose LH surge does not reach the kit’s threshold may get false results
- Women who experience mini LH peaks before the real LH surge may receive false results from the ovulation kit, which leads them to have intercourse earlier than they should and lower their chances of pregnancy.
- Women with short luteal phases may miscalculate when to use the test, as the ovulation kit’s prediction is based on an average-length luteal phase. In other words, in women with short luteal phases, the kit may indicate anovulation where in reality the ovulation has not yet occurred!
- Women with irregular cycles will receive invalid results, as the kit’s range covers only 5 to 9 days. For example, a woman with a cycle of 24 to 40 days, her ovulation ranges from day 10 to 26, which is a range of 16 days, much longer than the kit’s range.
- The kit does not provide any information about the cervical fluid. Although it might estimate the correct time of ovulation, the cervical fluid may not be suitable for transmitting the sperm to the egg for fertilization.
- If the kit is not held in proper conditions and is exposed to excessive heat during delivery or storage, its accuracy and reliability may be compromised.
- The kit’s results will be invalid if the women are on:
- Fertility drugs containing FSH, LH or HCG
- Antibiotics containing tetracycline
- Hormone therapy
- The kit’s results will probably be invalid if the women are
- Pregnant
- Postpartum
- Breastfeeding.
Other Options Of Ovulation Prediction
These three ovulation detection devices discussed below are more accurate than the common ovulation prediction kits, but still, they do not provide any information about your cervical fluid or waking temperature. Charting your key fertility signs is still the best way to boost your fertility and maximize your chances of conception!
Clearblue Fertility Monitor
This palm-size electronic device measures the levels of LH and estrogen in your urine and estimates if you are currently in your low, high or peak phase of your cycle. It can determine your ovulation one to two days before it occurs and notify you a number of days before. However, the results may be compromised if you:
- Are in menopause
- Are or have recently been pregnant
- Are breastfeeding
- Suffer from PCOS
- Have impaired liver or kidney function
- Use certain drugs (antibiotics containing tetracyclines, hormonal treatments, Clomiphene citrate, fertility treatments containing hCG or LH)
OvaCure Fertility Monitor
This device includes a handheld monitor with two sensors, an oral and vaginal sensor, which collects information about your cycle. Every day you place the oral sensor on your tongue for a few seconds and the sensor measures changes in the electrolyte levels in your saliva which are affected by estrogen. The monitor will then display the trends in a color-coded calendar and identify your Optimal Fertility Day, and alert you 5 to 7 days before impending ovulation so you can plan intercourse accordingly. The vaginal sensor detects when you have switched from estrogen dominance to progesterone dominance, which indicates that ovulation has indeed occurred.
The oral in combination with the vaginal sensor can estimate your possible ovulation and can also work for women with PCOS or irregular cycles, as they do not depend on LH levels.